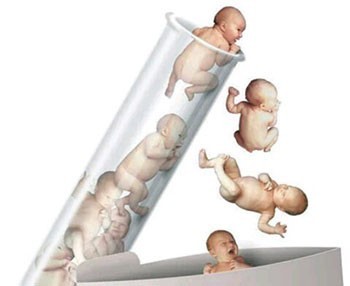
Fertility and IVF

IVF IN TURKEY
The first test tube baby was born in our country, 11 years after the first application in the world, and Turkey's first test tube baby was born on April 18, 1989. From this date until the end of the 1990s, it remained a treatment method that could only be performed in a few hospitals in big cities such as Istanbul, Ankara and Izmir and was not known by the society.
The fact that infertility is generally accepted as a taboo among the people, due to the structure of Turkish society, played a major role in this situation. Since the beginning of the 2000s, it is now defined as a giant sector where more than 45,000 couples are treated annually, with the investments of the private sector and the involvement of the media.
In cases where the egg and sperm cells cannot come together and the embryo formation or the embryo attached to the uterus cannot be achieved due to a reason that is present in the male, female and sometimes both of the couples, the said cells are taken out of the body and kept in the laboratory. We can summarize as obtaining embryos and transferring embryos to the uterus with the aim of creating pregnancy.
Assisted reproductive techniques (ART) are in vitro fertilization IVF and microinjection or intracytoplasmic sperm injection ICSI. The only difference between them is in the way of fertilization. In the microinjection (ICSI) method, the sperm is inserted directly into the egg with the help of a micropipette. With the introduction of ICSI, the chance of curing infertility due to male problems has increased considerably. Methods called TESE and TESA are used in men who do not have sperm in their semen or in cases where there is sperm production but cannot be expelled. In TESA, in cases where the ducts of the man are clogged and he cannot get the sperm out, tissue is removed from the man's testis with a needle and the egg is fertilized with the sperm obtained from it. In TESE, a piece is taken directly from the testis. At this stage, sperm is searched, and when TESE is performed using a microscope, it is called microTESE. In this method, the chance of finding sperm is higher and the testicle is less damaged.
TREATMENT STAGES
IN WHICH SITUATIONS, IVF CAN BE DONE?
• Couples who could not get pregnant despite 3 vaccination attempts
• Double-sided occlusion of the tubes • Ovulation sloth –
• In women who have widespread adhesions in the abdomen due to chocolate cyst (ENDOMETRIOMA-ENDOMETRIOSIS) and pregnancy cannot be achieved with treatment
• In cases where sperm counts are low or absent or sperm functions are severely impaired
• Unexplained infertility (In cases where pregnancy cannot be achieved with other treatment methods)
• History of recurrent pregnancy loss • Decreased number of eggs in women
• In Some Hormonal Disorders
• In order to diagnose some hereditary diseases at the embryo stage and to obtain a healthy baby (with pre-contamination genetic diagnosis methods) TREATMENT STAGES STAGE
1 “FINDING THE CAUSE OF INfertility by EVALUATION OF THE COUPLE” STAGE
2 “Stimulation of the ovaries”
3. STAGE: “COLLECTING EGGS AND CREATING EMBRYO” STAGE
4 “DEVELOPMENT AND SELECTION OF EMBRIOS FOR TRANSFER”
5. AND FINAL STAGE “EMBRYO TRANSFER”
There is an explanation of the stages in this bottom part, but it is too long to put it on the web address. I added it in order to create an individual idea about this process. The process is long and they go a little too far in terms of contacting the physician.
1.STAGE . “FINDING THE CAUSE OF INfertility by EVALUATION OF THE COUPLE”
The first and most important step in IVF treatment is to correctly identify the factor or factors that cause infertility and to plan the appropriate treatment for the solution. Because in some cases, a problem that is correctly detected can be solved with much easier and low-cost approaches (for example, surgical operation) before the in vitro fertilization application. This stage primarily includes the detailed examination and examination of men and women by specialist physicians. A point that should not be forgotten is that about half of the patients who apply to IVF centers in the world and in our country with the aim of having a child have a male or female problem. In approximately 25%, problems can be detected on both sides. In addition, the source of the problem cannot be determined exactly, although further examinations are performed in 20% of our couples who apply. These cases are called "unexplained infertility".
STAGE 2 “Stimulation of the ovaries”
If the appropriate treatment is planned as a result of the necessary examinations and analyzes, the second stage is to ensure the development of an appropriate number of eggs for treatment by applying external hormone therapy. At this stage, which is called ovulation induction among doctors, it is aimed to develop more than one egg cell by applying certain drug regimens. Although some protocols are frequently used among specialist physicians, drug doses may need to be adjusted individually for successful ovulation induction, and the same dose of drugs may have extremely different results in different people and therefore in different metabolisms. For this reason, developing the necessary and sufficient number of eggs without disturbing the physiology of the female individual in IVF treatments really requires experience and knowledge. Hormone drugs are used to stimulate the ovaries. For this, suppressive hormones are used for about two weeks. The person can apply these hormones to the subcutaneous area by himself. Following suppressive treatment, the menstruating patient is called on the 3rd day of menstruation, evaluated with blood tests and ultrasonography, and hormonal drugs are started to stimulate egg development, while folic acid and zinc supplementation is given to prevent possible defects in the nervous system of the fetus. In addition, short-term antibiotic therapy is given to patients as needed. The purpose of these procedures is to increase the chance of pregnancy by obtaining a large number of eggs and then a large number of embryos. The drug doses and duration used may be different for each patient. This woman's age is determined by the number of eggs, blood hormone levels, responses to previous treatments, and height/weight ratio. The most frequently applied protocols are short, ultra-short, antagonist, and long protocols. Which of these will be applied is decided at the first examination. After the drugs are started, blood and ultrasound examinations are performed at regular intervals to monitor the egg development, this may take approximately 10-14 days. When the desired egg size and uterine inner wall (uterine wall) thickness is reached, a cracking injection is made and the egg collection process begins 34-36 hours after that. However, there is a situation that should not be ignored. Not every follicle called an egg on ultrasound contains an egg. Especially in patients with 1-2 eggs (follicle) seen on ultrasound, eggs may not be obtained in the egg collection process. Sometimes the opposite happens, and in patients with multiple follicles, more eggs than expected may be obtained, since not all of them can be counted on ultrasound. In another case, it is the fertilization rate of the eggs. This rate is 70-80% on average. In other words, 7-8 out of 10 eggs are fertilized. However, in some rare cases, none of the eggs are fertilized and the transfer process does not occur. This situation is double explained and the transaction is cancelled.
THIRD STAGE: “COLLECTING EGGS AND CREATING EMBRYO”
The third stage is the stage of collecting the developed egg cells in the second stage in the operating room environment when the maturation period is completed, evaluating the eggs taken in the laboratory environment, and combining them with the sperm cells taken from the same day for the fertilization process.
Egg retrieval (OPU- Oocyte pick up) is a procedure performed vaginally with the help of a needle attached to the Ultrasonography (USG) probe 34-36 hours after the injection of the egg cracking needle. Local or general anesthesia can be applied. If general anesthesia will be applied, the patient should not eat or drink anything after 24 hours the previous night. Each follicle in the ovaries is emptied one by one with the help of a needle, accompanied by vaginal USG, and taken into sterile tubes. The follicle fluid in the tubes is examined under the microscope in the embryology laboratory and it is investigated whether there is an egg in it. If the egg is not found in the first time, the follicle is washed by giving fluid to the follicle again, and the egg search is continued by evacuating it again. After the egg is found, it is passed to other follicles. Egg collection takes about 10-30 minutes. Sometimes there is no harm in taking appropriate painkillers, as groin and abdominal pain may occur. Minor bleeding and infections may occur rarely. If the number and quality of sperm cells taken from the spouse is suitable for fertilization of the eggs obtained, these eggs and sperm cells are placed in the same container in the embryology laboratory and the fertilization of the egg by the best quality sperm is ensured, just as in a normal pregnancy. If the sperm cells obtained are not suitable for this process in terms of number, motility and quality, then it is ensured that the selected sperm cells are injected into the eggs one by one using the method called microinjection. In some cases, when sperm cells are not found in the semen sample taken from the spouse, sperm cells are obtained from the tissues taken from the male ovaries (testes) and used in microinjection. From the moment the egg and sperm cells are taken, they are kept in special liquids in the laboratory environment and in technological devices called an incubator, in an environment similar to the body environment (providing a certain temperature and gas ratio). About 16-18 hours after this process, that is, in the morning of the next day, fertilization checks of the eggs are made in the laboratory. The genetic material from both the male and female forms two progenitor nuclei in the egg. This structure is defined as normal fertilization and they are taken into the incubators where they are grown again to follow the advanced embryo development stages. Approximately 70% of the egg cells taken in a standard IVF procedure and considered mature form normal fertilization. Of course, this rate may vary depending on the reasons for infertility of the couples, the age of the patient, and the quality of the egg and sperm cells used.
PHASE FOUR “DEVELOPMENT AND SELECTION OF EMBRIOS FOR TRANSFER”
With the fourth stage,the couples are happy and then one step closer. At this stage, fertilized embryos are grown with the help of special fluids and devices, as mentioned above, in a way similar to the physical conditions in the maternal reproductive system, and the best embryo is selected. In a normal pregnancy, the embryo, which develops approximately 4 or 5 days after the egg and sperm cells come together and fertilization occurs, now comes to the stage of attachment to the uterus and pregnancy. Embryos obtained in IVF laboratories are grown in a similar way, and their daily development is followed, and the embryo or embryos with the highest chance of attaching to the uterus during this period are selected by experienced specialists with the utmost care. According to the results of the treatment, if more good quality embryos are obtained than the number to be transferred, these embryos can be frozen and stored for five years and can be used to achieve pregnancy again when certain conditions are met within this storage period.
FIFTH AND FINAL STAGE “EMBRYO TRANSFER”
The fifth stage consists of the selection of the embryo with the highest pregnancy potential, and then the transfer of the selected embryo to the mother's womb with the help of a special catheter, and it can be said that it is the most important step of the treatment. Because, no matter how high-quality an embryo is obtained, it is the most important key for a successful treatment to carry out embryo transfer by creating minimal trauma to the uterus of the embryo and without disturbing the environment in which the embryo will attach to the uterus as much as possible. During this procedure, a factor that is present in the uterine environment or that may occur due to treatment may lead to failure of the result, no matter how high quality embryos are transferred. For this reason, even at a low rate, the embryo transfer process is delayed in some treatments, the embryos obtained are frozen and the transfer is performed when the uterine environment becomes suitable for the embryo to attach. Embryo transfer can be done any day from day 2 to day 5 after fertilization. The day on which the transfer will be made is decided by considering the embryo quality, the number of developing embryos, the age of the patient, and whether a genetic diagnosis is made or not. In cases where the embryo quality is good and the number of embryos is high, the 5th day transfer is performed if the patient's age is appropriate. The transfer process is short-term and painless.


